Reducing Medication Errors for Healthcare Providers
Healthcare is a field where precision is non-negotiable. One area where accuracy critically matters is medication administration. Lapses in this area can lead to medication errors, potentially causing severe patient harm or even fatal outcomes. However, numerous evidence-based strategies can significantly reduce the prevalence of such errors, fostering patient safety and trust in healthcare organizations.
Medication errors are preventable, and implementing strategic measures to combat them should be a priority for every healthcare facility, be it a hospital setting, an emergency department, or an intensive care unit. Evidence-based strategies have proven their worth by drastically reducing errors in medication administration, ensuring patient safety, and improving patient outcomes.
At every step, patient safety is always the primary consideration. The end goal is to ensure that healthcare systems globally can administer medications safely and accurately – every time.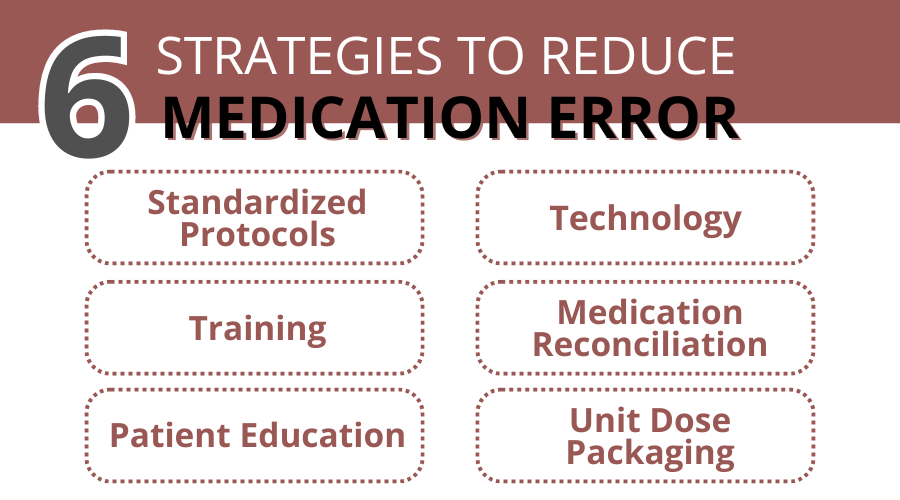
Evidence-Based Strategies: A Systematic Review
Having addressed the importance and impact of medication errors in the healthcare field, it is crucial to comprehend and effectively implement evidence-based strategies to curb these errors. Understanding systematic reviews and literature reviews of various scientific studies can help.
A systematic review, as the name suggests, systematically collects, critically appraises, and synthesizes research on a clearly defined research question. In our context, that question focuses on medication error reduction strategies. The goal is to provide a large-scale overview of what the existing medical literature says on this topic.
Some of the most impactful evidence-based recommendations include:
- Use of Standardized Protocols and Checklists: Standardized guidelines can reduce the risk of confirming biases or forgetting crucial steps during medication administration. This can significantly decrease the chances of a medication error.
- Technological Advancements: Electronic systems like electronic health records (EHRs) or computerized physician order entry (CPOE) can streamline the process of medication administration and limit the opportunity for human error.
- Medical Team Training and Simulation: Regular team-based simulations can enhance inter-professional communication and improve health professionals’ preparedness for high-risk, high-stress situations, where medication errors often occur.
- Medication Reconciliation: This strategy involves obtaining a comprehensive list of a patient’s medications and comparing them with the current list in use. It avoids drug-drug interactions and ensures correct doses and routes of administration.
- Patient Education and Involvement: Empowering patients to be active participants in their care can also be a line of defense against medication errors.
- Unit Dose Medication Packaging: Unit dose packaging ensures medications are contained in single-unit packages in a ready-to-administer dose and form. According to ASHP, unit dose systems are “(1) safer for the patient, (2) more efficient and economical for the organization, and (3) a more effective method of utilizing professional resources”
These strategies lay the foundation for a proactive and organized approach to medication safety. Each of these strategies, when implemented thoughtfully and consistently, has been shown to trigger a significant reduction in medication errors.
Case Studies: Implementing Strategies in Diverse Healthcare Settings
Having poured over systematic reviews and research, we must observe how these evidence-based strategies play out in real-world healthcare settings. Whether it is in a high-pressure emergency department or a bustling hospital setting, the implementation of these strategies has shown remarkable results. Here are a few case studies that demonstrate the successful application of these strategies.
1. Hospital Setting
This is a qualitative study aimed at identifying strategies to prevent medication errors in hospital wards in Iran. The study involved interviews with 16 nurses and 1 physician, focusing on two main themes: “acting professionally” and “presenting technical strategies.” The results emphasized the importance of professional behavior, such as:
- Reading drug labels carefully
- Continuous training
- Awareness of legal issues related to medication errors
Technical strategies included distinguishing high-risk medications and keeping certain medications separate. The study concludes that a combination of professional conduct and technical strategies can significantly reduce the incidence of medication errors and adverse events in hospitals.
2. Emergency Department:
This study evaluated the impact of implementing bar-code medication administration (BCMA) in a community hospital emergency department on medication errors and nursing satisfaction. The medication error rate dropped from 2.96% to 0.76%, a 74.2% relative reduction. The study concluded that barcode implementation in the emergency department effectively reduced medication errors from adverse drug events and even enhanced nursing satisfaction.
3. Intensive Care Unit (ICU):
According to the Science Direct medication administration error in pediatric care units research, medication errors “are more likely to occur in critical care settings due to the fast-paced environment and patient vulnerability.” The interventions in this study included:
- Raising awareness
- Reinforcing closed-loop medication administration systems
- Enhancing compliance with independent double-checks
- Updating the drug library
- Introducing electronic order sets
As a result of these safe medication practices, the medication error rate dropped significantly, achieving a rate of zero errors per 1,000 patient days by the first quarter of 2022. The study highlights the importance of a collaborative approach and the use of technology to improve patient safety in critical care settings.
These case studies highlight the considerable improvements in patient care, safety, and overall health outcomes achievable by applying evidence-based strategies.
The Role of Technology in Preventing Medication Errors
Modern healthcare has increasingly turned towards technology to push the boundaries of patient care. When it comes to reducing medication errors, technology has proven to be a valuable ally. From digitizing patient records to automating prescription filling, technological advancements offer promising ways to streamline processes and reduce the scope for human error.
Electronic Health Records (EHRs) have transformed the way healthcare providers track patient history and medication schedules. By having all information organized and instantly accessible by the right people, EHRs help eliminate errors due to incomplete patient information or poor communication between healthcare professionals.
In an age of electronic systems, electronic prescribing systems play a key role in reducing prescription errors. By offering automatic checks for issues like drug-drug interactions and allergies, they provide an added layer of safety.
Barcoding technology allows healthcare workers to customize medication labels to include all essential information in an organized database. Medical Packaging Inc’s Pak-EDGE barcoding software is designed to streamline the process of designing customized labels and barcodes for prescription drug products, this software helps eliminate one of the significant causes of medication errors – mislabeling.
With today’s technology progressing at uncharted speeds, we can expect more innovations to play an increasingly vital role in preventing medication errors.
The Long-Term Impact of Reduced Error & How MPI Can Help
Not only can these strategies enhance the safety of patients, but they also contribute to the reduction of healthcare costs and the improvement of the overall health system. Each correctly administered medication signifies a victory in maintaining and restoring health.
Yet, the application of evidence-based strategies is no small task. This transformative process requires dedication, resources, and, often, the adoption of robust technological systems. That is where Medical Packaging Inc. (MPI) can help.
MPI offers a full range of medication packaging equipment including unit dose packaging machines and barcode labelers to facilitate the prevention of medication errors. Our Pharmacy Accessory Label Printer (PALP) prints accurate barcoded labels to affix on ampoules, vials, and oral syringes, reducing room for errors and increasing medication administering efficiency.
Our Pak-EDGE UD Barcode Labeling Software facilitates organization by streamlining the process of creating customized labels and barcodes for your vast array of prescription drug products and accessories.
At MPI, our goal aligns with yours – minimizing medication errors and safeguarding patient health. We are dedicated to aiding healthcare facilities like yours in accomplishing this mission with our innovative products and tailored solutions.
It is evident that a multi-faceted approach combining evidence-based strategies with efficient technological solutions offers a promising path. By combining the powers of technology and innovation, we can ensure medication safety in every healthcare setting.
Contact us today or request a free quote to see how our products can significantly reduce the risk of medication error in your healthcare facility.
Resources:
Author links open overlay panelEmmanuel Aoudi Chance a, et al. “The Effectiveness of Checklists and Error Reporting Systems in Enhancing Patient Safety and Reducing Medical Errors in Hospital Settings: A Narrative Review.” International Journal of Nursing Sciences, Elsevier, 8 June 2024, www.sciencedirect.com/science/article/pii/S2352013224000577.
Hamad, Meshaal Mohammed Eisa, and Sulaiman Bah. “Impact of Implementing Electronic Health Records on Medication Safety at an HIMSS Stage 6 Hospital: The Pharmacist’s Perspective.” The Canadian Journal of Hospital Pharmacy, U.S. National Library of Medicine, 3 Oct. 2022, www.ncbi.nlm.nih.gov/pmc/articles/PMC9524548/.
D’Angelo, Anne-Lise. “Error Management Training in Medical Simulation.” StatPearls [Internet]., U.S. National Library of Medicine, 24 July 2023, www.ncbi.nlm.nih.gov/books/NBK546709/.
Barnsteiner, Jane H. “Medication Reconciliation.” Patient Safety and Quality: An Evidence-Based Handbook for Nurses., U.S. National Library of Medicine, www.ncbi.nlm.nih.gov/books/NBK2648/. Accessed 3 Aug. 2024.
Kim, Yoon-Sook, et al. “Can Patient and Family Education Prevent Medical Errors? A Descriptive Study.” BMC Health Services Research, U.S. National Library of Medicine, 31 Mar. 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7106564/.
Unit Dose Drug Distribution, www.ashp.org/-/media/assets/policy-guidelines/docs/statements/unit-dose-drug-distribution.pdf. Accessed 13 Aug. 2024.
Author links open overlay panelAlireza Salar, and AbstractBackground and purposeAdministering drugs is one of the primary nursing acts in hospital wards and medication errors are one of the worst errors among nurses leading to unpleasant results for patients. Thus. “Preventing the Medication Errors in Hospitals: A Qualitative Study.” International Journal of Africa Nursing Sciences, Elsevier, 10 Aug. 2020, www.sciencedirect.com/science/article/pii/S2214139120301128.
Author links open overlay panelKelly Owens PharmD, et al. “The Effect of Implementing BAR-Code Medication Administration in an Emergency Department on Medication Administration Errors and Nursing Satisfaction.” Journal of Emergency Nursing, Mosby, 19 Sept. 2020, www.sciencedirect.com/science/article/abs/pii/S009917672030235X.
Author links open overlay panelZahra Ghezaywi a b 1, et al. “Targeting Zero Medication Administration Errors in the Pediatric Intensive Care Unit: A Quality Improvement Project.” Intensive and Critical Care Nursing, Churchill Livingstone, 14 Dec. 2023, www.sciencedirect.com/science/article/pii/S0964339723002136.
Contact MPI Today for Personal Assistance
MPI’s Drug Master File provides speed-to-market regulatory and technical support related to our packaging components for medical and pharmaceutical market clients